Assessing Pain

Pain is often called the fifth vital sign. In conjunction with temperature, pulse, blood pressure, pain can reveal a tremendous amount about the health status of the patient. Pain also affects the quality of life through its affect on such things as mood, activity, appetite, sleep, hygiene, and the ability to focus and concentrate. Pain is subjective and nurses and other members of the healthcare team depend on the patient's report to determine how to treat the pain.
Pain Control
To achieve adequate pain control, it is necessary to understand how to assess pain. Pain is totally subjective, and what causes excruciating pain to one person, may only be perceived as moderate pain to someone else. This is why nurses need to dig deep to understand the patient's pain and how to best help alleviate it.
Assessing Pain
Nurses use methods such as PQRST to assess a patient's pain and with healthcare the team determine the plan of care to achieve pain control.
The PQRST method examines several key factors in the pain process.
P= Provocation or Palliation
What causes the pain? how did it start? What makes it better and what makes it worse?
Q= Quality/Quantity
Describe the pain using words such as sharp, dull, aching, excruciating, stabbing, burning, throbbing, nauseating, shooting, twisting, crushing.
R= Region/Radiation
Where is the pain? Does it stay in one place or does it radiate elsewhere or move around?
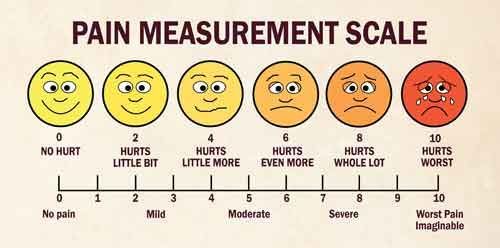
S= Severity Scale
Using a scale of 0-10 (see below) where would the patient rate the pain using 0 as no pain and 10 as the worst pain ever? What's the current level? What was the worst rating in the past 24 hours? How long does it last? Does it interfere with sleep, activity, eating?
T= Timing
When (time) did the pain start? How long does it last? How often does the patient have this pain? What was the patient doing just before the pain began? Is it worse at night or in the day time? Is the pain accompanied by other symptoms such as nausea/vomiting, diarrhea, dizziness, lightheadedness?
Assessment Tools
There are several pain assessment tools used by health care professionals to help assess pain levels. These may include the Wong-Baker Faces Pain Rating Scale which depicts several faces from a smiling face representing no pain to a face depicting tears and a scowl representing the worst pain imaginable.
Verbal Pain Scale
A verbal pain scale uses colors from blue to red and a series of vertical lines stretching from blue representing no pain to deep red representing severe pain.
Numerical Pain Scale
The numerical pain scale, uses a scale from 0 to 10; where 0 represents no pain and 10 represents the worst pain imaginable.
In addition to the pain scales, health care professionals need to ask questions to determine the quality of the pain and how it affects your functioning. These include:
How does the pain affect the patient's life:
It is important to understand that medications will not cure pain or eliminate it. Medications work in many ways to help ease pain such as by changing how your brain perceives the pain, by improving flexibility, by treating underlying factors causing pain, or by reducing inflammation or swelling.
Medications are designed to affect specific types of pain receptors in the brain. Understanding the cause of the pain helps determine what kind of pain medication will work best. And then educating the patient in how and why this should work. If it doesn't, then further investigation may be needed to determine a more accurate rating and cause. Pain medication should be used for short term duration with a plan for weaning off of them.
Non-pharmaceutical measures as appropriate should be used in combination such as ice, heat, compression, elevation, rest, massage, acupuncture, acupressure, range of motion, mild activity, stretching. The type and duration or frequency will be dependent upon the cause of the pain. Consult with the MD and educate the patient in safety and need to incorporate these measures into the plan. This is even more important in light of the Opioid Addiction Crisis.
Documentation
Careful documentation provides the healthcare team the best possible ongoing assessment of the pain and measures that work or don't to improve the comfort level or alleviate the pain.
It's essential to remember pain is subjective. Some people have no pain tolerance and others can tolerate a lot before they think to complain. Additional symptoms or illness can also affect the patient's tolerance. But what the patient perceives is what you need to document. If you have reason to suspect the patient may be exaggerating the rating, document behavior and activity that you observe.
It's also important to be able to document how well the patient understands the pain scale used. Patients with dementia are not always reliable in reporting pain accurately. You may need to question his family or caregivers about his response to pain. Is his judgement being clouded due to medication or excruciating pain. If the patient is also experiencing symptoms such as nausea or vomiting, this may affect the ability to report.
The patient should also be asked about what level of pain is acceptable at this time. Expect the tolerance to vary. and manage the pain control plan accordingly.
Observe and ask about the effectiveness of pain medications or other non-pharmaceutical measures and document the outcomes.
A verbal pain scale uses colors from blue to red and a series of vertical lines stretching from blue representing no pain to deep red representing severe pain.
Numerical Pain Scale
The numerical pain scale, uses a scale from 0 to 10; where 0 represents no pain and 10 represents the worst pain imaginable.
In addition to the pain scales, health care professionals need to ask questions to determine the quality of the pain and how it affects your functioning. These include:
- Where is the pain?
- When did it start?
- What makes it worse?
- What helps to ease it?
- Is it sharp, dull, aching, throbbing, shooting, burning?
How does the pain affect the patient's life:
- Sleep patterns
- Eating
- Activity patterns
- Your mood and emotions
- Is it affecting family life and relationships?
- Does the pain affect physical appearance, sexual function, energy levels, ability to work?
It is important to understand that medications will not cure pain or eliminate it. Medications work in many ways to help ease pain such as by changing how your brain perceives the pain, by improving flexibility, by treating underlying factors causing pain, or by reducing inflammation or swelling.
Medications are designed to affect specific types of pain receptors in the brain. Understanding the cause of the pain helps determine what kind of pain medication will work best. And then educating the patient in how and why this should work. If it doesn't, then further investigation may be needed to determine a more accurate rating and cause. Pain medication should be used for short term duration with a plan for weaning off of them.
Non-pharmaceutical measures as appropriate should be used in combination such as ice, heat, compression, elevation, rest, massage, acupuncture, acupressure, range of motion, mild activity, stretching. The type and duration or frequency will be dependent upon the cause of the pain. Consult with the MD and educate the patient in safety and need to incorporate these measures into the plan. This is even more important in light of the Opioid Addiction Crisis.
Documentation
Careful documentation provides the healthcare team the best possible ongoing assessment of the pain and measures that work or don't to improve the comfort level or alleviate the pain.
It's essential to remember pain is subjective. Some people have no pain tolerance and others can tolerate a lot before they think to complain. Additional symptoms or illness can also affect the patient's tolerance. But what the patient perceives is what you need to document. If you have reason to suspect the patient may be exaggerating the rating, document behavior and activity that you observe.
It's also important to be able to document how well the patient understands the pain scale used. Patients with dementia are not always reliable in reporting pain accurately. You may need to question his family or caregivers about his response to pain. Is his judgement being clouded due to medication or excruciating pain. If the patient is also experiencing symptoms such as nausea or vomiting, this may affect the ability to report.
The patient should also be asked about what level of pain is acceptable at this time. Expect the tolerance to vary. and manage the pain control plan accordingly.
Observe and ask about the effectiveness of pain medications or other non-pharmaceutical measures and document the outcomes.
